“I thought I was just getting older,” Mark, a 45-year-old teacher, told me in clinic. For months he woke up tired and went to bed exhausted. When we tested, it wasn’t age—it was hepatitis C.
Here’s the truth I want you to remember: hepatitis C early symptoms are often subtle, but recognizing them can change the entire course of your health. When we find the virus early, treatment today is short, highly effective, and can prevent long-term damage.
For a broader view of preventive health, explore our Complete Guide to Preventive Health.
Table of Contents
What Is Hepatitis C—and Why Is It So Quiet?
Hepatitis C is a blood-borne virus that targets the liver. It spreads through infected blood—most commonly from sharing needles or equipment for injection drug use, medical exposures before the early 1990s (when screening improved), or unregulated tattoos and piercings. Left unchecked, it can lead to cirrhosis (scarring), liver failure, or liver cancer.
Doctors sometimes call it the “silent infection” because the liver is resilient and keeps working even under attack. That means hepatitis C early symptoms can feel like everyday issues—until they don’t.
The CDC recommends one-time screening for all adults, with periodic testing for people with ongoing risk factors. Learn more at the CDC’s hepatitis C page (https://www.cdc.gov/hepatitis/hcv/).
The First Warning Sign Most People Miss: Fatigue That Doesn’t Lift
If I could highlight one hallmark of hepatitis C early symptoms, it’s profound, lingering fatigue. Not the “stayed up too late” kind—this is bone-deep exhaustion that sticks around despite rest.
Why it happens:
- Inflammation from the virus puts your immune system on high alert.
- A taxed liver struggles to filter byproducts, so more “waste” circulates in your bloodstream, leaving you foggy and drained—like a slow-motion flu.
How it feels different from regular tiredness:
- It lasts for weeks or months.
- Patients describe it as “walking through molasses.”
- It can come with mild nausea, sore joints, and a drop in appetite.
Quick Self-Check: Are These Familiar?
Use this simple scan if you’re worried about hepatitis C early symptoms:
- Fatigue that doesn’t improve with sleep
- Sore joints without a clear cause
- Occasional nausea or upset stomach
- Reduced appetite and “brain fog”
These alone don’t prove hepatitis C—but together, especially if you have risks, they’re a nudge to get tested.
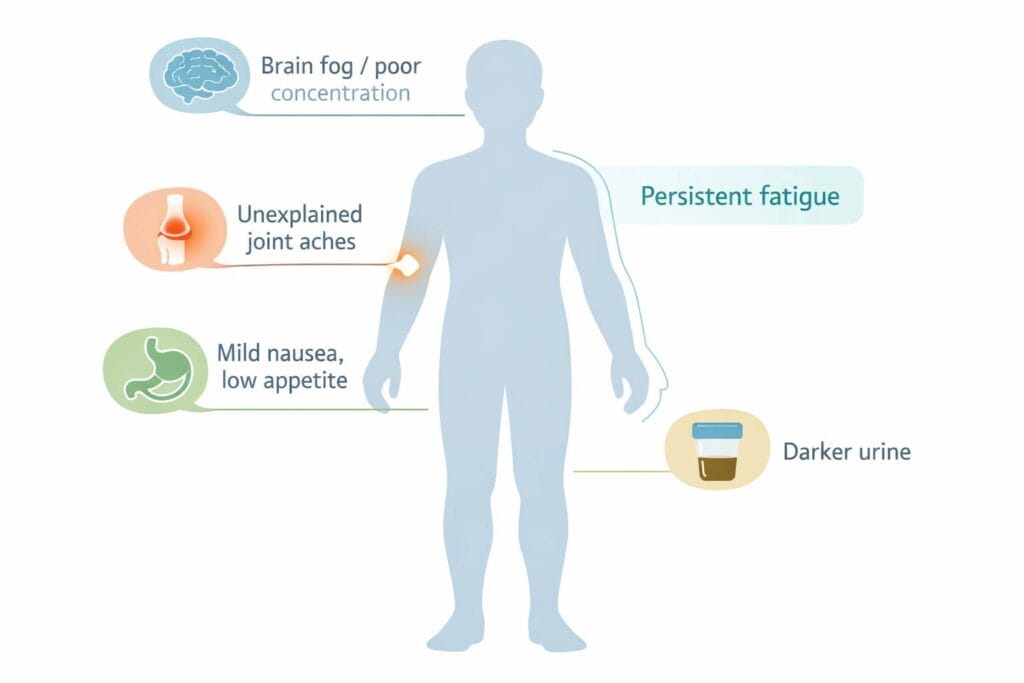
Hepatitis C Early Symptoms to Watch For
Fatigue is common, but it’s not the only early clue. Other subtle signs include:
- Darker urine (sometimes tea-colored)
- Light, gray, or clay-colored stools
- Itchy skin without an obvious rash
- Mild tenderness in the upper right abdomen (where the liver sits)
- Low mood or concentration dips not tied to clear stressors
These symptoms can be caused by many conditions. The point is not to self-diagnose—but to use them as a prompt to have a conversation with your clinician.
Is It Normal Tiredness—or Something More?
Below is a practical comparison I share with patients. It’s not a diagnosis tool, but it can help you decide when to call your doctor.
| Feature | Everyday Tiredness | Hep C–Related Fatigue |
|---|---|---|
| Duration | Improves in days with rest | Persists for weeks or months |
| Quality | Sleepy, recover after weekend | Heavy, “wading through mud” |
| Companions | Stress, busy week | Brain fog, mild nausea, joint aches |
| Urine/Stool changes | Unchanged | Darker urine, pale stools possible |
Why These Signs Are Easy to Ignore
Many of us chalk fatigue up to long hours, poor sleep, or simply “getting older.” Hepatitis C early symptoms rarely include sharp pain, so people adapt to feeling 10–20% worse and keep pushing. That quiet creep is why testing matters: some untreated cases progress to cirrhosis over time. Testing early lets us act early.
Who Should Consider Testing?
Even if you feel well, screening is a smart move. Consider testing if you:
- Ever shared needles or equipment for injection drug use—even once
- Had a blood transfusion or organ transplant before 1992
- Got a tattoo or piercing in an unregulated or non-sterile setting
- Work in healthcare and had a needlestick
- Have been on long-term hemodialysis
- Were born to a mother with hepatitis C
Guidance at a glance:
| Group | Why Risk Rises | Testing Recommendation | Next Step |
|---|---|---|---|
| All adults | Silent infection is common | One-time screening | Ask PCP for HCV antibody test |
| Ongoing injection drug use | Blood exposure risk | At least annually | Plan regular follow-up testing |
| Pre-1992 transfusion | Older blood screening | One-time screening now | Confirm status with PCR if positive |
| Healthcare needlestick | Occupational exposure | Per employer protocol | Report exposure immediately |
How Testing Works—and What Results Mean
If hepatitis C early symptoms resonate with you, testing is straightforward:
1) HCV antibody test: Shows if you’ve ever been exposed. It’s a simple blood test.
2) HCV RNA (PCR) test: If the antibody is positive, this confirms whether the virus is active.
Good news: Direct-acting antiviral medications cure more than 95% of active hepatitis C infections, often in 8–12 weeks, with few side effects for most people.
Practical Steps You Can Take Today
If you suspect hepatitis C early symptoms, don’t panic—act.
- Schedule testing with your primary care clinician or local clinic. Many community programs offer confidential, low-cost testing.
- Protect your liver now:
- Avoid alcohol completely; it accelerates liver damage.
- Aim for a balanced diet: leafy greens, whole grains, lean proteins, healthy fats.
- Stay hydrated and move daily—walking counts.
- Check medications and supplements with your clinician to avoid liver strain.
- Keep a symptom diary. Note fatigue levels, appetite, any urine/stool changes, and mood.
Real-World Example: Catching It Early
A few months after treatment, Mark told me, “It’s like someone turned the lights back on.” His energy returned gradually, then decisively. That’s the promise of early detection: the sooner we identify hepatitis C early symptoms and confirm the diagnosis, the faster we can help you feel like yourself again—and protect your liver for the long run.
Honest Answers to Common Questions
- Can hepatitis C go away by itself? Some people clear the virus spontaneously in the first six months, but most develop chronic infection without treatment. Testing clarifies where you stand.
- Is it safe to exercise? Yes—light to moderate activity is generally beneficial. Listen to your body and discuss specifics with your clinician.
- What about cost? Many health plans cover testing and modern treatment. Patient assistance programs exist—ask your care team or pharmacist to help you apply.
- Can I spread it to family? Hepatitis C is spread through blood. It is not spread through casual contact, hugging, or sharing food. Avoid sharing razors, toothbrushes, or anything that may have blood on it.
Authoritative source: WHO hepatitis C factsheet (https://www.who.int/news-room/fact-sheets/detail/hepatitis-c).
Key Takeaways You Can Act On
- Fatigue that lingers for weeks—especially with brain fog, low appetite, or subtle digestive changes—is worth a conversation with your doctor.
- Even without symptoms, universal one-time screening is recommended for adults. Testing is quick and reliable.
- Treatment today is short, well-tolerated, and cures most people—protecting your liver and your future.
If anything here sounds familiar, bring it up at your next visit. You’re not overreacting—you’re taking a smart, proactive step for your health.
A Closing Note
Your body whispers before it shouts. Hepatitis C early symptoms can be quiet—but they’re meaningful. A 10-minute test can give you clarity, and if needed, a proven path to cure. If you’re on the fence, consider this your gentle nudge: get screened, feel reassured, and move forward with confidence.
Disclaimer: This article is informational and not a substitute for medical advice. Please consult your clinician for personal recommendations.